| I’m a regular MedCityNews reader, just to follow the latest developments in eHealth and ‘Obama care’. Although I haven’t been able to track the original study, I was quite interested to read about a three month diabetes patient empowerment trial, showing quite interesting outcome results. Even more interesting is the 'willingness to pay' part of the study. Being triggered on this line of thought, I remembered hearing about positive results in a similar Belgian cardiovascular tele-rehabilitation study in the news a few weeks ago. The ‘Telerehab III’ study was easy to find and frankly, the results are astonishing. Not only because they also show very positive outcome results, but because the mobile health intervention has a clearly ‘dominant’ cost-effective effect. Are we deaf, dumb and blind ? Why don’t we dig much deeper in this obvious goldmine of health ?
Why do companies continue to invest billions in a drugs for some rare diseases and omit to spend a fraction of that amount and a much shorter time to develop simple and highly cost-effective ‘mobile health – patient empowerment’ tools ? MedCityNews
I cite this week’s MedCityNews editorial (and regret not having been able to find the original study yet; it might be the mDAWN project that was referred to):
A three-month experiment with bimonthly text messages, a Web portal and home-based medical devices produced an average weight decrease of 3.5 pounds and a mean reduction in haemoglobin A1c levels from 7.41 to 6.77 percent. (NB: anything below 7 percent indicates good control of Type 2 diabetes). Participants received Wi-Fi blood-pressure monitors and weight scales, to upload data automatically to a secure website. They also self-reported blood-glucose levels from monitors they already had. Patients and their caregivers could see the same data trends as the clinicians managing their diabetes. They also received health tips and reminders through a portal and via text messaging, as well as access to a semi-facilitated discussion board with other members of the study group. At the end of the three months, all participants rated the program favourably, and a 56 percent said they would be willing to foot the bill for the technology, about $100 up front and $20 a month for on going service. “They saw value because they felt empowered, healthier and more in control of their lives by the increased self-awareness; many created self-care routines and habits from the data and feedback their received”, Kendall Ho (director of the eHealth Strategy Office at the University of British Columbia in Vancouver) said. “This new sense of self-confidence carried over into their expectations of future interactions with their doctor, as patients noted that they were now able have a more knowledgeable conversation and were more confident in knowing which questions to ask. In essence, participants felt they were now more ‘activated’ patients who would be more involved in making decisions about their care with their doctors.”
The Belgian YorBody platform
Two years ago I looked at the possibility to start distributing the Limburg mHealth tool YorBody in pharmacies. It’s a accelerometer, combined with an app on your smartphone and a common digital platform, originally designed for cardiovascular rehabilitation (after heart surgery and bypass operations). This platform can also be used for an practically unlimited number of purposes to motivate patients to move, get up a flight of stairs again, walk around the block every day, exercise more or even learn to run a marathon in six months. Just to give you an idea of the ‘investment’ needed: I was looking at promoting this platform trough the pharmacies that participated in the P4F (Prepare for the Future) training, I was giving at that time. It would cost patients / users something like €30 the first month (this fee would include the provision of the specific accelerometer, installing the app, logging on to the platform and choosing the appropriate exercise program) and a monthly subscription of somewhere between €10 and €5 (depending on the number of months one would pay up front). Telerehab III
What could you achieve with this kind of money? Just read what the Telerehab III study revealed:
Background: Notwithstanding the cardiovascular disease epidemic, current budgetary constraints do not allow for budget expansion of conventional cardiac rehabilitation programs. Consequently, there is an increasing need for cost effectiveness studies of alternative strategies such as tele-rehabilitation. The present study evaluated the cost effectiveness of a comprehensive cardiac tele-rehabilitation program. Design and methods: This multi-centre randomized controlled trial comprised 140 cardiac rehabilitation patients, randomized (1:1) to a 24-week tele-rehabilitation program in addition to conventional cardiac rehabilitation (intervention group) or to conventional cardiac rehabilitation alone (control group). The incremental cost-effectiveness ratio was calculated based on intervention and health care costs (incremental cost), and the differential incremental quality adjusted life years (QALYs) gained. Results: The total average cost per patient was significantly lower in the intervention group (€2156±€126) than in the control group (€2720±€276) (p=0.01) with an overall incremental cost of €–564.40. Dividing this incremental cost by the baseline adjusted differential incremental QALYs (0.026 QALYs) yielded an incremental cost-effectiveness ratio of €-21,707/QALY. The number of days lost due to cardiovascular rehospitalisations in the intervention group (0.33±0.15) was significantly lower than in the control group (0.79±0.20) (p=0.037). Conclusions: This paper shows the addition of cardiac tele-rehabilitation to conventional centre-based cardiac rehabilitation to be more effective and efficient than centre-based cardiac rehabilitation alone. These results are useful for policymakers charged with deciding how limited health care resources should best be allocated in the era of exploding need.
Dominant cost-effectiveness
New treatments have to show a positive ICER (Incremental Cost-Effectiveness Ratio) . This is the extra cost per quality adjusted (really healthy) life year. That’s the definition of a QALY. If you’re not familiar yet with health-economic concepts, read Lieven Anneman’s excellent book about this subject. 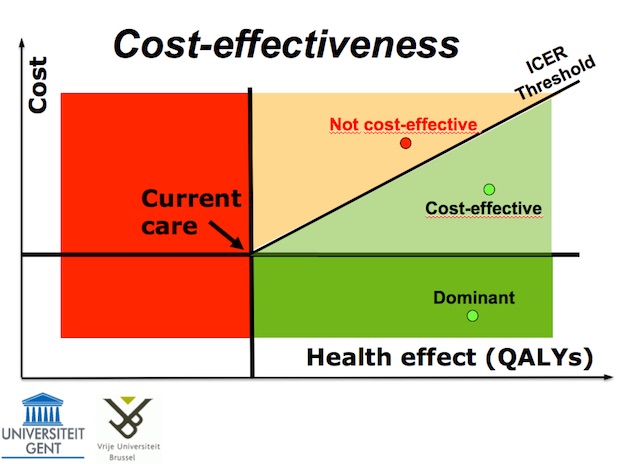
To be considered "cost-effective", new treatments have to stay in the light green area, below the ICER threshold. But even those who cost €16.000 per QALY gained get reimbursed. It is rare that a new treatment winds up in the dark green, ‘dominant’ area.
That means that you can win QALY’s while spending LESS money.
And strangely enough, that’s exactly what both studies above prove. Are we deaf, dumb and blind ?
The question is : what is keeping us from digging deeper in this goldmine of health ? Why can’t we see the obvious health and cost benefits ? Why don’t we invest in developing these simple mHealth tools ? Why don’t we define and open up the necessary standardised, safe, high quality data- and knowledge platforms ? - Is it because it's too easy ?
- Or that it is unfamiliar ground we will be walking on ?
- Or that it will empower patients (who will no longer be patiently waiting for us to help them, but will rather start helping themselves) ?
- Or that some / most of this stuff is no longer ‘exclusive’ or patentable and therefor not lucrative enough to put a lot of money in ?
My prediction is that the obvious is not going to stay invisible much longer. Sooner, rather than later, some kind of ‘Ryan Air-’ or 'Uber'-like stakeholder will come and change healthcare forever. mHealth and the kind of applications that are described above, will be at the heart of this revolution. We better start investing and developing ourselves, if we don’t want to wind up like the larger or smaller traditional players like PanAm or Sabena, that no longer fly the skies. Dirk BROECKX – 28 November 2015 |